Angioplasty
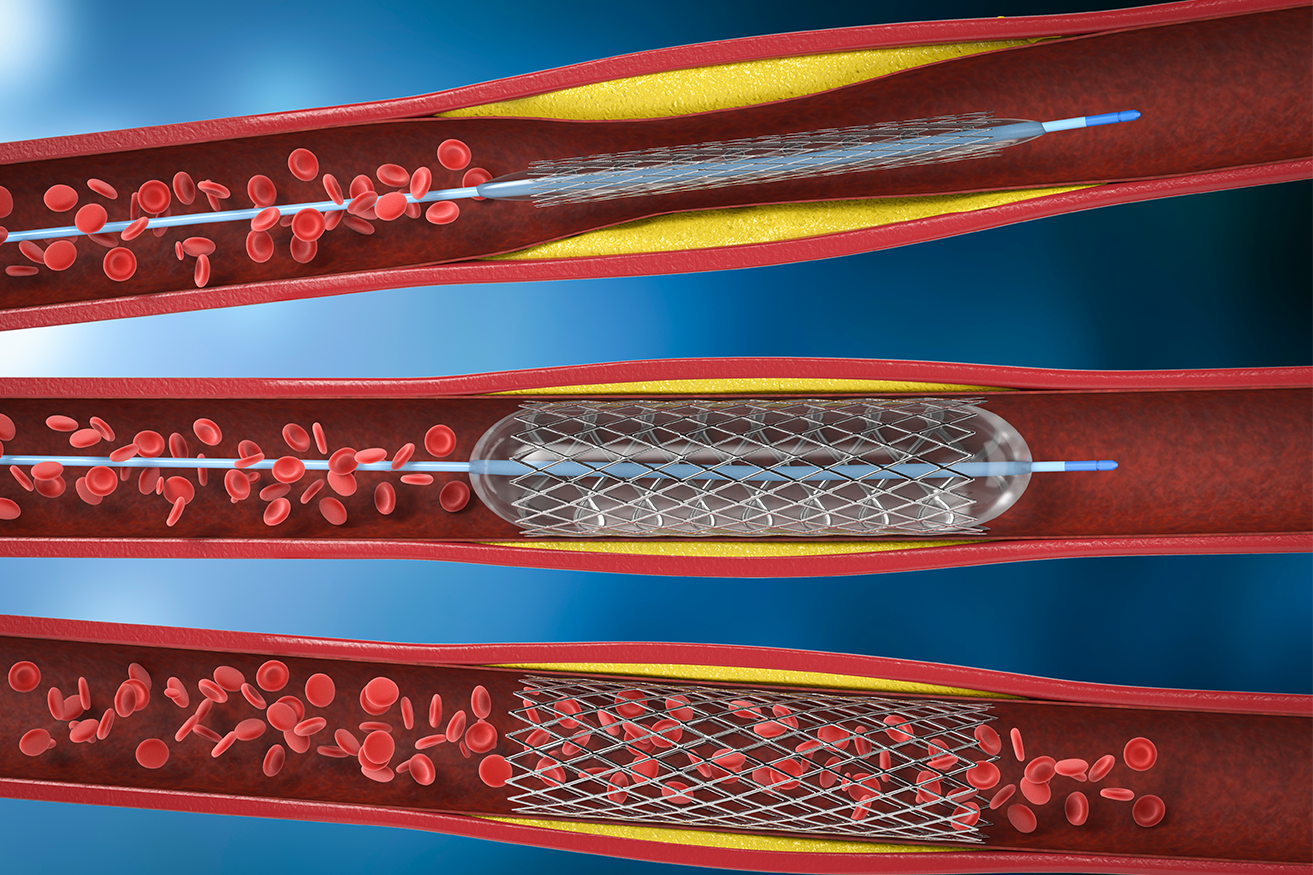
Coronary angioplasty (AN-jee-o-plas-tee), also called percutaneous coronary intervention, is a procedure used to open clogged heart arteries. Angioplasty uses a tiny balloon catheter that is inserted in a blocked blood vessel to help widen it and improve blood flow to the heart. Angioplasty is often combined with the placement of a small wire mesh tube called a stent. The stent helps prop the artery open, decreasing its chance of narrowing again. Most stents are coated with medication to help keep the artery open (drug-eluting stents). Rarely, bare-metal stents are used. Angioplasty can improve symptoms of blocked arteries, such as chest pain and shortness of breath. Angioplasty is also often used during a heart attack to quickly open a blocked artery and reduce the amount of damage to the heart.
-
Why it's done
Angioplasty is used to treat the buildup of fatty plaques in the heart’s blood vessels. This buildup is a type of heart disease known as atherosclerosis.
Angioplasty may be a treatment option for you if:
- You have tried medications or lifestyle changes but these have not improved your heart health.
- You have chest pain (angina) that is worsening.
- You have a heart attack. Angioplasty can quickly open a blocked artery, reducing damage to your heart.
Angioplasty isn’t for everyone. Depending on the extent of your heart disease and your overall health, your doctor may determine that coronary artery bypass surgery is a better option than angioplasty for you.
You may need coronary artery bypass surgery if:
- The main artery that brings blood to the left side of your heart is narrow.
- Your heart muscle is weak.
- You have diabetes and multiple severe blockages in your arteries.
In coronary artery bypass surgery, the blocked part of your artery is bypassed using a healthy blood vessel from another part of your body.
-
Risks
Although angioplasty is a less invasive way to open clogged arteries than bypass surgery is, the procedure still carries some risks.
The most common angioplasty risks include:
- Re-narrowing of your artery: When angioplasty is combined with drug-eluting stent placement, there’s a small risk the treated artery will become clogged again. The risk of re-narrowing of the artery is higher when bare-metal stents are used.
- Blood clots: Blood clots can form within stents even after the procedure. These clots can close the artery, causing a heart attack. It’s important to take aspirin in combination with clopidogrel (Plavix), prasugrel (Effient), or another medication that helps reduce the risk of blood clots exactly as prescribed to decrease the chance of clots forming in your stent.
Talk to your doctor about how long you’ll need to take these medications. Never stop taking these medications without discussing it with your doctor.
Bleeding: You may have bleeding in your leg or arm where a catheter was inserted. Usually, this simply results in a bruise, but sometimes serious bleeding occurs and may require a blood transfusion or surgical procedures.
-
How you prepare
Before a scheduled angioplasty, your doctor will review your medical history and do a physical exam. You may need to have some tests, including a chest X-ray, electrocardiogram and blood tests, before your procedure. Your doctor will also perform an imaging test called a coronary angiogram to see if the arteries to your heart are blocked and if they can be treated with angioplasty.
If your doctor finds a blockage during your coronary angiogram, he or she may decide to perform angioplasty and stenting immediately after the angiogram while your heart is still catheterized.
Your doctor will give you instructions to help you prepare.
1)Your doctor may instruct you to adjust or stop taking certain medications before angioplasty, such as aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners. Be sure to tell your doctor about all medications you take, including herbal supplements.
2) Usually, you’ll need to stop eating or drinking six to eight hours before an angiography.
3) Take approved medications with only small sips of water on the morning of your procedure.
4) Gather all of your medications to take to the hospital with you, including nitroglycerin, if you take it.
5) Arrange for transportation home. Angioplasty usually requires an overnight hospital stay, and you won’t be able to drive yourself home the next day. -
Results
Coronary angioplasty greatly increases blood flow through the previously narrowed or blocked coronary artery. Chest pain generally should decrease. You may be better able to exercise.
Having angioplasty and stenting doesn’t mean your heart disease goes away. You’ll need to continue healthy lifestyle habits and take medications as prescribed by your doctor.
If you have symptoms similar to those you had before coronary angioplasty, such as chest pain or shortness of breath, contact your doctor. If you have chest pain at rest or pain that doesn’t respond to nitroglycerin, call 911 or emergency medical help.To keep your heart healthy after angioplasty, you should:
1) Quit smoking
2) Lower your cholesterol levels
3) Eat a healthy diet that is low in saturated fat
4) Maintain a healthy weight
5) Control other conditions, such as diabetes and high blood pressure
6) Get regular exercise
7) Take medications as prescribed by your doctor
8) Successful angioplasty also means you might not have to undergo coronary artery bypass surgery, a more invasive procedure that requires a longer recovery time.